When Is It Safe to Play Again After a Sports-Related Brain Injury?
Are you or a loved one recovering from a sports-related brain injury? Studies show that approximately 15% of all trauma injuries reported in high school sports are traumatic brain injuries (TBIs). After such injuries, when can you return to the field or court?
An alternative to dealing with the injury using conventional medical treatments is taking a holistic or whole-body approach to regenerate, heal and cultivate well-being.

While recovering at home, a reliable WiFi connection for online games may also help enhance brain recovery. Research shows that playing video games may provide cognitive benefits.
Sports and Traumatic Brain Injury
Sports participation is one of the primary causes of brain injury among individuals 15 to 24 years old. The sports world has taken steps to help prevent TBI and permanent brain damage.
It is essential to know the difference between head trauma and TBI. For example, a head injury is any trauma to the skull, scalp, or brain.
One potential indicator of TBI is when a person experiences an alteration in mental status. Following a sports-related head injury, a medical examination can determine whether a TBI or concussion has occurred.
A concussion refers to a TBI that affects one’s brain function. The effects are typically temporary. However, they can include headaches and issues with concentration, memory, coordination, and balance.
An athlete should remain cautious following a head injury as it may include brain injury. This process involves not returning to play on the day of the head injury.
A medical practitioner should conduct a cursory examination and order tests to determine whether a TBI has occurred.
After a doctor performs a basic examination, medical professionals should conduct more detailed evaluations and order testing such as magnetic resonance imaging (MRI).
Such tests can provide a baseline of the athlete’s brain function. Various functions to examine include attention, memory, and problem-solving.
Such neurocognitive testing can provide a basis for pre- and post-injury testing.
Sports Teams’ Concussion Protocols
Following a sports-related head injury, a physician’s post-concussion monitoring may include:
- Presence or absence, and period of loss of consciousness
- Period of posttraumatic memory loss
- Persistence of symptoms
Some team physicians may conduct a 5-minute series of questions known as the Standardized Assessment of Concussion (SAC). SAC is part of some concussion protocols.
Meanwhile, the Immediate Post-Concussion Assessment and Cognitive Test (ImPACT) is a computer-based testing program designed to manage sports-related concussions.
Levels of Sports-Related Head Injuries
Athletes who experience head injuries may experience other injuries besides concussions.
Here is a sample sports-related head injury grading system. It identifies a head injury’s severity and provides a timetable for returning to sports participation safely.
Grade 1: Mild physical trauma to the athlete’s head, such as a bump, laceration, or contusion.
Grade 2: Characterized by migraine-like headaches with related symptoms
Grade 3: Mild TBI characterized by:
- An immediate change in mental status
- Loss of consciousness for under one minute
- Amnesia for less than 30 minutes
Grade 4: TBI that may include:
- Loss of consciousness for over one minute and under five minutes
- Amnesia for over 30 minutes but under 24 hours
Grade 5: Severe TBI, which may be life-threatening. Symptoms of Grade 5 injuries may include:
- Physical brain injuries
- Bleeding within the brain
- Increased intracranial pressure. The cranium is composed of cranial bones that surround and protect the brain.
- Unconscious for over five minutes
- Amnesia for over 24 hours
Standard Neurological Testing Options for Brain Injuries
Physicians may order various tests to provide a diagnosis based on the above head injury grading system:
Glasgow Coma Scale (GCS)
This test is to establish:
- Baseline level of consciousness
- Motor function
- Eye function
Patients receive scores ranging from 3 to 15 on the GCS. Higher scores indicate less severe brain injuries.
Periodic evaluations are needed to determine the patient’s neurologic improvement or deterioration.
Computerized Tomography (CT scan)
This test provides immediate data about a person’s status following a head injury. The primary function of CT scans is to rule out an enormous mass lesion that may be compressing the brain.
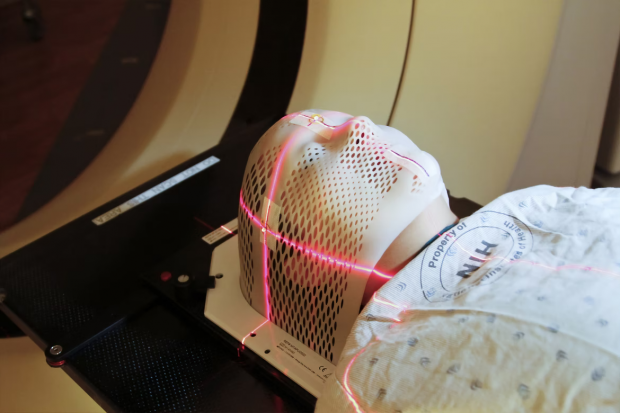
Magnetic Resonance Imaging (MRI)
MRIs allow doctors to view subtle changes that a CT scan may not capture.
Return-to-Play Guidelines
Here are some sample guidelines that team physicians can follow to determine whether players who have experienced a TPI are medically ready to return to play.
Grade 1: Athletes may return to play if the physical injury has healed
Grade 2: Athletes may return to play if asymptomatic (no symptoms) and have completed a team’s or league’s return-to-pay (RTP) protocol.
Players with Grade 2 injuries or higher should also undergo neurocognitive testing following the injury. They may resume play after injury-related symptoms are resolved when compared with baseline testing.
Grade 3: Players may participate in any sports activities that can result in head trauma. In addition, they must be asymptomatic and complete the five-day RTP activity protocol.
Following four injuries, a neurologist or neurosurgeon must provide clearance before RPT is permitted.
Grade 4: A break should follow each incidence of head injury.
First injury: 30 day-break
Second injury: 90-day break
Third injury: 180-day break
RTP may be allowed if athletes are asymptomatic. The players must also receive favorable results from neurocognitive testing compared to the baseline.
Grade 5: Athletes may return to play after six months following an MRI. The MRI should show no structural damage within the brain.
This stipulation includes athletes who remained unconscious for over five minutes or over one day but produced normal results from a neurologic exam.
Athletes should not return to play in particular situations. They include MRIs indicating evidence of a concussion or other sign of abnormality, or the neurologic exam is still abnormal.
Tips to Help Prevent Head and Neck Injuries in Contact Sports
If you are into contact sports, such as football, rugby, and hockey, here are some tips to help prevent head and neck injuries.
- Ensure that you receive sufficient strengthening and preconditioning of the head and neck muscles.
- Ball-carriers should avoid lowering their heads when contacting a tackler.
- Get pre-season physical exams. You and your team should identify players with prior concussions or other brain or spinal injuries.
- Physicians and trainers should ensure players’ equipment is fitted properly, including the helmet.
- The team’s entire staff should be prepared for possible spinal cord injuries.
- Coaches and officials should discourage players from using the top of their helmets offensively when hitting, blocking, or tackling. Such actions should be disallowed during practice and games.
Final Thoughts
Today, TBI has justifiably become a public health concern in the sports world.
It’s critical for team players, coaches, trainers, physicians, and owners to understand the severity of brain injuries in sports medicine.
While many players return to play after concussions and other TBIs, staying on the sideline and the side of caution is always a practical option. The game of life is too precious.
References
1. Head Injuries: When Is It Safe to Return to Play?
https://brighamhealthhub.org/sports-related-head-injuries-when-is-it-safe-to-return-to-play/
2. Traumatic brain injury
https://ksi.uconn.edu/emergency-conditions/traumatic-brain-injury/
3. Cognitive benefits of playing video games
https://www.arapahoe.edu/blog/cognitive-benefits-playing-video-games
4. Concussion
https://www.mayoclinic.org/diseases-conditions/concussion/symptoms-causes/syc-20355594
5. Sports-related Head Injury
https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Sports-related-Head-Injury
6. Head injury – first aid
https://medlineplus.gov/ency/article/000028.htm
7. Cranium
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cranium
